Assessing Needs and Planning Person-centred Care
Report outlining the stages of the nursing process as applied to Roy’s care. The role of assessment models (RLT) and care approaches (person-centred care) in this focusing on one aspect of Roy’s care.
Introduction & Background to the Service User
The Nursing and Midwifery Council's (2018) Future Nurse proficiency standards emphasise that nurses have a critical role in assessing and planning patient care. This report discusses the Nursing Process and the Roper-Logan-Tierney Model of Nursing to assess and plan patients’ care as applied to Roy, a former police officer in his sixties who retired following two myocardial infarctions. Roy is a type 2 diabetic patient with multi-morbidity including rheumatoid arthritis, peripheral vascular disease, neuropathy in his feet, and depression, requiring a nurse to show him how to use his blood glucose monitor. The appointment presented an opportunity for a full patient's needs assessment.
The Nursing Process
Historically, the "medical model" focused on diagnosing and treating patients based solely on their physical symptoms, ignoring their concerns, relationships, and psychological well-being (Hamilton and Price, 2013). For example, a patient with gangrene of a limb would have removed the part affected overlooking the effects to the patient’s life. Yura and Walsh insisted on the need for a problem-solving approach in nursing care, proposing, the nursing process: Assessment, Planning, Implementation, and Evaluation, known as APIE. Although this systemic process remains fundamental to determine the healthcare needs of patients and plan personalised care (Melin-Johansson et al., 2017), scholars have argued expanding APIE (Yildirim and Ozkahraman, 2011) so to include nursing Diagnosis after Assessment and Re-check preceding Evaluation. The result was ASPIRE: Assessment, Diagnosis, Planning, Implementing, Re-check, Evaluation.
To better understand the nursing process, we will discuss the key stages of the extended model ASPIRE. Assessment is the first stage of the nursing process. The nurse must well execute the assessment for the nursing process to work. Hamilton and Price (2013) stated that this is the most critical part of learning the patient's needs. It involves getting to know the patient while gathering subjective and objective information (Bickley et al., 2020). While subjective information involves the patient, their family and carers’ concern and views, objective information is actual data measured through observations such as vital signs, weight, and test results. Data can be gathered in many ways and sources including the patient or caregivers. Friends can also help by giving important information and using electronic patient records can facilitate the assessment. Once the Assessment is completed, a nursing Diagnosis can be made. This is an additional step to the initial APIE which The American Nurses Association (2017) defined as the second standard of practice. In this stage, the nurse analyses all the data obtained to identify current and prospective problems (Yildirim and Ozkahraman, 2011). After determining issues and risk factors and forming a nursing hypothesis, the nurse can establish a diagnosis used to set a care plan. After the nursing diagnosis, the planning stage identifies actions to mitigate, resolve, or prevent issues while building on the person’s strengths (Ellis et al., 2020). To identify care priorities, one must consider the severity and patient's requirements before setting goals with the patient. To provide a clear direction, motivation, and focus for everyone involved, Ravello and Fields (2015) recommend using SMART goals, meaning setting specific, measurable, achievable, realistic, and timely goals. The care to be implemented must be stated in detail in the action planning. Hogston (2011) suggests adopting the six REEPIG criteria, meaning that the care plan must be: realistic, explicit, specified clearly without leaving room for misunderstandings, evidence-based, prioritised according to the most critical issues, and goal-centred such that the planned care meets the aim. After the nurse and the patient agree the care plan, Implementing is the stage where the patient receives treatments. Rechecking is the other additional step that helps the nurse and patient determine whether the interventions are working before the final stage of the process, Evaluation. This is critical to a favourable outcome. When healthcare professionals intervene or provide treatment, they evaluate and verify the intended result (NICE, 2021). The nursing process is an essential tool for putting nursing knowledge into practice and is a systematic problem-solving method to determine healthcare needs and provide quality and personalised care.
Although the nursing process sets the standard of nursing care, some barriers could impede the success of the process (Ellis et al., 2020); nurses must learn how to recognise and overcome barriers. For example, interruptions during assessments delay care and result in mistakes or omissions. The most effective way to overcome this while assessing a patient is to provide privacy before beginning the assessment. Another barrier is patient anxiety, which makes gathering information challenging. It can alter vital signs, which could be misinterpreted. By making the patient comfortable and keeping a calm approach, anxiety can be reduced. As a result, it will help maintain the standard of care the process sets. One primary obstacle to adopting the nursing process is the lack of information and awareness among nurses regarding the execution of the process and a lack of assistance from management systems, resulting in nursing education experts introducing complementary models to help mitigate these challenges.
Assess
Hamilton and Price (2013) defined Assessment as a pillar of the nursing process; therefore, its correct and broad execution is essential and the models of nursing and living, introduced by Nancy Roper, Winifred W. Logan, and A. J. Tierney aimed to guide, and structure this part of the nursing process (Holland and Jenkins, 2019). Although they targeted students to help them become familiar with the nursing approach, these concepts are now used throughout the United Kingdom and Europe (Holland and Jenkins, 2019). The five key concepts are (Roper et al., 2006):
12 Activities of Daily Living
Lifespan
Dependence/Independence continuum
Factors Influencing the Activities of Living
Individualising Nursing.
The RTL Model of Nursing identified 12 Activities of Daily Living:
Maintaining a Safe Environment
Communication
Breathing
Eating and Drinking
Elimination
Washing and Dressing
Controlling Temperature
Mobilisation
Working and Playing
Expressing Sexuality
Sleeping
Death
Lifespan spans from birth to death and is divided in five periods: "infancy, childhood, adolescence, maturity, and senior citizenship" (Roper et al., 2006), recognising that not everyone reaches all five throughout their lifetime (Holland and Jenkins, 2019). Each of the twelve activities of daily living is affected by the life stage (Ellis et al., 2020). For instance, infants are more reliant and require different care than adults. However, adulthood does not ensure independence. An adult who is unconscious is a clear example of it: because of his condition, he will need help with almost all daily tasks. The Dependence/Independence continuum has close connections with the Activities of Daily Living and Lifespan. One must assess the patient's ability to execute the activities individually for reliance and autonomy. Each activity is evaluated as a patient gains autonomy or dependence. Moreover, daily life activities are often interrelated, meaning independence in one may suggest a similar outcome in another. For instance, a loss of movement post-surgery may lead to becoming more reliant on maintaining a safe environment and eliminating and needing assistance in washing and dressing and reaching the toilet safely. The same is true for dependency. Another concept that the model identifies is the factors that affect how people execute their living activities. The biological factorlooks at the patients' overall health and how their anatomy and physiology are affected. The psychological factor highlights the effects of emotions, ideas, spiritual beliefs, and the capacity to comprehend things. Thesociocultural component refers to the effect of society and culture on the individual patient. The sociocultural element comprises expectations and beliefs based on class, status, and culture. In other words, it refers to the individual patient's beliefs, expectations, and aspirations for themselves and those of others regarding independence and the ability to carry out everyday tasks (Holland and Jenkins, 2019). One should consider the effect that the surrounding conditions have on the activities of living and vice versa. The final factor is the political-economic, which refers to how governmental policies and economic conditions, such as programmes, funding, and reforms, influence daily activities (Holland and Jenkins, 2019). Influential factorsare essential when assessing a patient as they affect every aspect of a person's life, Hamilton and Price (2013) say that they reveal the person’s individuality.
To understand how the preceding four concepts interact to shape personality, we turn to individuality. Individuality in life is how a person experiences and behaves based on their preferences, abilities, and beliefs. Each activity is checked for typical abnormalities before continuing. After assessing a person's activities of living, the nurse can detect actual and potential complications with daily life activities and develop an individualised care plan using the nursing process. Actual problems need solutions, whereas prospective problems demand prevention (Holland and Jenkins, 2019), leading to personalised care that will help the patient transition from dependence to independence. Individualising nursing acknowledges the patient as an individual deserving respect and dignity.
The concept of individualising nursing strongly relates to person-centred care, and as described by NHS England (2016), it helps people acquire the understanding, confidence, and skills to effectively manage and make informed decisions about their health and care. Additionally, it ensures that patients are treated with dignity, compassion, and respect. Health and social care professionals collaborate with service users to coordinate and tailor care as needed (Dowrick, 2017).
The Health Foundation (2014) has identified person-centred care with a four-principles framework:
1. Treating people with dignity, compassion, and respect.
2. Providing coordinated care, assistance, or treatment.
3. Delivering personalised care, assistance, or treatment.
4. Supporting patients to identify and develop their strengths and abilities to live an independent and fulfilling life. Regardless of the type of care or intervention, healthcare professionals should always follow these principles. (NHS England, 2016).
In Roy's case, it is critical to acknowledge his difficulties and help him find possible solutions. For example, he describes medical jargon as a foreign language used by healthcare professionals. This can confuse and diminish understanding between healthcare professionals and patients in patient care. To improve collaborative practice and high-quality care for Roy, we must avoid using acronyms and unfamiliar medical terminology to ensure that all team members understand what we have said, as well as patients and their families (NICE, 2014). This will make the patient feel more in control and allow him to live more independently without relying on his wife to do research to try and understand.
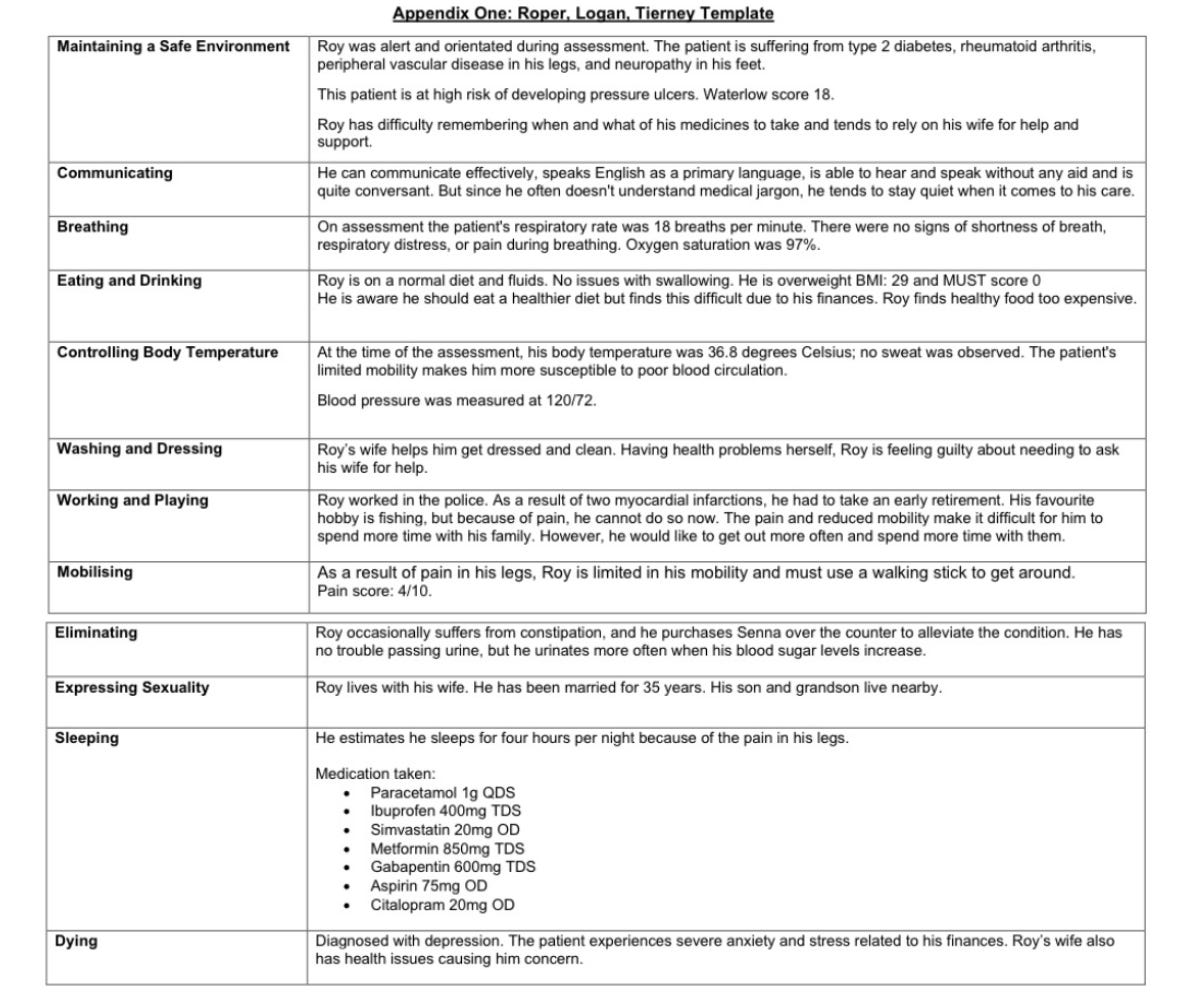
See Appendix One
Systematic Nursing Diagnosis
Roy's initial nursing diagnosis has highlighted a risk for uncontrolled blood glucose resulting from inadequate monitoring and an unhealthy diet, as indicated by no weight loss and frequent urination. Additionally, depression and psychological degradation are indicators of powerlessness in relation to the chronic condition and dependence on his wife. Because of the devastating consequences that high glucose levels can have on people, such as nerve damage responsible more than 160 amputations every week in England alone (NHS England, 2020), the priority is the management and control of his blood glucose levels. The nursing priority is to assist the patient with managing his diabetes and keeping it under control to prevent complications and health deterioration. Priorities will change as the patient's needs change, and the nurse identifies evolving needs (NICE, 2021).
Plan/Implement/Recheck/Evaluate
A key component of person-centred care is shared decision making (SDM), which ensures that people have the support they need to make the right decisions (The Health Foundation, 2014). It is a process in which a clinician works with a patient to help them decide on their treatment (Riding et al., 2017). As stated by the National Institute for Clinical Excellence (2021), the essential parts of shared decision making are recognising that a decision needs to be made, knowing and understanding the relevant evidence, and including the patient's preferences and values in the decision. During the discussion, clinicians draw on their expertise, as well as evidence, risks, benefits, and the knowledge of the patient, including his or her preferences, personal circumstances, goals, values, and beliefs (Riding et al., 2017). Patients whose care decisions adequately reflect their personal preferences often experience better results (NICE, 2021). So, shared decision making is an essential part of person-centred care.
In drawing up Roy's care plan to maintain blood glucose at a satisfactory level, we must make sure he knows how to use his new blood glucose monitoring machine, as checking blood sugar is an essential aspect of living with diabetes (Diabetes U.K.). It will help the patient understand if he needs to take more medication, eat something, or when he wants to get up and move around more. Furthermore, diet, food choices, and maintaining a healthy body weight are the cornerstones of diabetes management (Diabetes U.K.). A 2% to 10% reduction of the individual's body weight can dramatically improve blood glucose levels (Diabetes U.K.). The patient will need help and advice about nutritional therapy, as well as encouragement to make changes to his diet and way of life.
In support, a meal plan should take Roy's dietary choices, habitual mealtimes, and finances into consideration. Therefore, a thorough analysis of his diet will identify his eating habits and lifestyle. Also, encouraging the patient to read labels will help him choose foods with a low glycaemic index, higher fibre content, and low-fat content (Diabetes U.K.). Additionally, diet education, behavioural therapy, group support, and ongoing nutritional counselling must be offered.
Although the care plan has simple, measurable goals, and agreed with Roy, there might be cases of poor compliance. However, rather than focusing on neglected behaviours, healthcare professionals must positively reinforce self-care behaviours performed on evaluation (NICE, 2014).
See Appendix two
Conclusion
The Nursing Process is a problem-solving approach to providing nursing care, supported by nursing models (Hamilton and Price, 2013). The RLT Model of Nursing guides nurses during the assessment stage. A thorough assessment is crucial to provide personalised, effective care. Personalised care requires the patient to take an active role in their care. Because of that, Shared Decision Making is essential of patient-centred care and ensure patients commitment. As evidence suggests, patients actively involved in their care have better outcomes and experiences (NICE, 2021).
Reference List
Abdelkader F.A. & Othman W.N.E. (2017) Factors Affecting Implementation of Nursing Process: Nurses' Perspective. Journal of Nursing and Health Science, vol. 6, no. 3, pp. 76-82.
American Nurses Association (2017) The Nursing Process http://www.nursingworld.org/EspeciallyForYou/What-is-Nursing/Tools-You- Need/Thenursingprocess.html (accessed May 11, 2022)
Bickley, L.S. et al., (2021) Bates' guide to physical examination and history taking, International; 13th ed., Wolters Kluwer, Philadelphia.
Ellis, P., et al., (2020) Patient assessment and care planning in nursing, 3rd edn., Learning Matters, London.
Diabetes U.K., Living with diabetes Diabetes U.K. (no date) Available at: https://www.diabetes.org.uk/guide-to-diabetes (accessed May 16, 2022).
Dowrick, C., (2017) Person-centred Primary Care: Searching for the Self, Taylor, and Francis.
Hamilton P. & Price T., (2013) The Nursing Process, Holistic Assessment and Baseline Observations. In: Brooker C, Waugh A (eds) Nursing Practice: Fundamentals of Holistic Care. Mosby Elsevier, London. 303-336.
Holland, K. & Jenkins, J., (2019) Applying the Roper-Logan-Tierney model in practice, 3rd edn, Elsevier, Edinburgh.
Hogston R., (2011) Managing Nursing Care. In: Foundations of Nursing Practice: Themes, Concepts and Frameworks. 4th ed. Palgrave Macmillan: London. pp. 2-21.
Melin‐Johansson, C., et al., (2017), Clinical intuition in the nursing process and decision‐making—A mixed‐studies review, Journal of clinical nursing, vol. 26, no. 23-24, pp. 3936-3949.
National Institute for Clinical Excellence. (NICE) What to expect during assessment and care planning, (2021) Available at: https://www.nice.org.uk/about/nice-communities/social-care/quick-guides/what-to-expect-during-assessment-and-care-planning (accessed May 16, 2022).
NHS England, (2016), Personalised care and support planning handbook: the journey to person-centred care: Core information, Available at: https://www.england.nhs.uk/wp-content/uploads/2016/04/core-info-care-support-planning-1.pdf (accessed May 20, 2021)
Nursing and Midwifery Council, (2018), Future nurse: Standards of proficiency for registered nurses, Nursing and Midwifery Council, London.
Riding, S., et al., (2017), Real-world challenges in delivering person-centred care: A community-based case study, British Journal of community nursing, vol. 22, no. 8, pp. 391-396.
Revello, K. & Fields, W., (2015), An Educational Intervention to Increase Nurse Adherence in Eliciting Patient Daily Goals, Rehabilitation nursing, vol. 40, no. 5, pp. 320-326.
The Health Foundation (2014) Person-centred care made simple. Available at: https://www.health.org.uk/publications/person-centred-care-made-simple (accessed May 16, 2022).
Yildirim B. & Ozkahraman S. (2011) Critical Thinking in Nursing Process and Education, International Journal of Humanities and Social Science. Vol. 1 No. 13 pp. 257-262.